Revisiting The Evidence For Breast Cancer Risk Reduction Following Removal Of Tubes And Ovaries In Patients With BRCA1 And BRCA2 Mutations
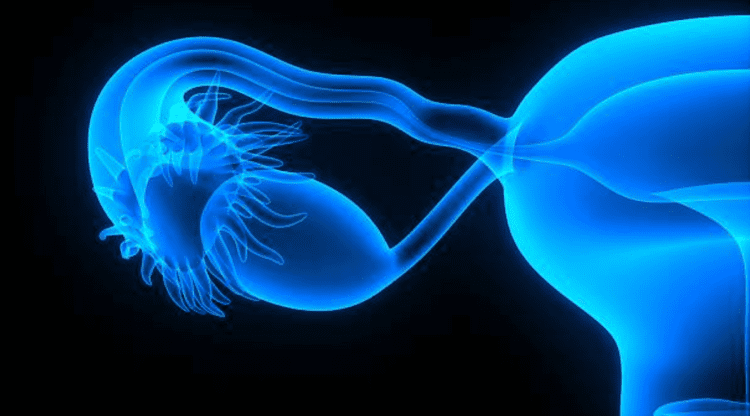 Within a short time after the discovery of the BRCA1 and BRCA2 breast/ovarian cancer genes in the mid-1990s two important facts came to light. First, was that removal of the ovaries impacted the risk of breast cancer as much as 50% in some series. The second fact was that many, if not most of the ovarian cancers arising from the presence of these genes actually arose in the fallopian tubes as opposed to the ovaries. The medical establishment addressed these findings in two ways. First, when there was a choice, prophylactic removal of the ovaries preceded breast removal. Furthermore, instead of removing just the ovaries, the fallopian tubes were removed as well.
Within a short time after the discovery of the BRCA1 and BRCA2 breast/ovarian cancer genes in the mid-1990s two important facts came to light. First, was that removal of the ovaries impacted the risk of breast cancer as much as 50% in some series. The second fact was that many, if not most of the ovarian cancers arising from the presence of these genes actually arose in the fallopian tubes as opposed to the ovaries. The medical establishment addressed these findings in two ways. First, when there was a choice, prophylactic removal of the ovaries preceded breast removal. Furthermore, instead of removing just the ovaries, the fallopian tubes were removed as well.
Recently, the degree of breast cancer risk reduction afforded by removal of the ovaries (oophorectomy) has been brought into question. In a recently reported study from multiple centers in Europe, Australia and New Zealand almost 4000 women tested positive for a BRCA1 or BRCA2 mutation. Between 30% and 40% of these women underwent prophylactic removal of the ovaries and tubes.
The study found no difference in breast cancer risk for those women with BRCA1 following removal of the ovaries and tubes. On the other hand, in patients who carried a BRCA2 mutation, removal of the ovaries resulted in a 32% reduction in breast cancer risk only when carried out before the age of 45. When the authors looked at the risk of breast cancer based on the time from oophorectomy, they noted that breast cancer risk reduction in BRCA2 patients was higher at 49%. Again, no obvious benefit was seen for patients with BRCA1 mutations.
Conclusions:
It is not surprising to see that removal of the ovaries has little to no impact of the breast cancer risk in patients with BRCA1 mutations and a substantial risk reduction in those with BRCA2 mutations. This is explained by noting that over 70% of those with BRCA1 mutations are estrogen receptor negative compared with only 30% of women with BRCA2 mutations. This new data is important when considering how to counsel patients carrying a gene mutation who are trying to decide whether to have tubes and ovaries or breasts removed first when considering prophylactic surgery. Those women with BRCA1 mutations might consider breast removal initially whereas those with BRCA2 mutations may benefit more from initially removing tubes and ovaries. As usual, things are not that simple as family history and age at diagnosis of cancer may impact greatly on these decisions. Your surgeon or genetics counselor may be quite helpful in this regard.